Shedding light on lesser-known and less common cancers
Published April 2025 | 5 min read
Expert contributor: Prof Winston Liauw, Medical Oncologist, Clinical Pharmacologist, member of HCF's Medical Advisory Panel and Director of the Cancer Services Stream for South East Sydney Local Health District
Words by Jo Hartley
Unlike breast and lung cancer, not all cancers are well known. But that doesn’t mean they’re any less important to know about.
In 2024, it’s estimated that around 169,000 cases of cancer were diagnosed in Australia. Less common cancers made up about 12% of this total. Less common cancers are defined as those that have between six and 12 cases per year, per 100,000 people.
“Less common cancers are generally difficult to detect early and that’s part of the reason why they’re not so well known,” says Professor Winston Liauw, Director of the Cancer Services Stream for South East Sydney Local Health District and member of HCF’s Medical Advisory Panel.
Less common cancers vs lesser-known cancers?
While some cancers are lesser known, there are also less common cancers. These are classified as:
- a form of a more common cancer
- located in an unusual part of the body
- found in a part of the body where cancer is rare (e.g. bones)
- more commonly found in the opposite sex (e.g. breast cancer in males)
- diagnosed in someone younger than typically expected (e.g. prostate cancer in someone under 40).
Currently, there are around 161 types of less common cancer, with the list often changing. Childhood cancer is considered rare, as it’s much less common than in adults, with about 760 Australian children diagnosed each year.
“More young people are being diagnosed with cancers now, especially bowel cancer," says Prof Liauw. "Liver cancer's also on the rise, driven by growing rates of liver disease linked to issues like diabetes and obesity.”
Happily, Prof Liauw says more people are living with cancer and getting treatment thanks to advancements and better accessibility. Yet, some cancers affecting Australians are simply not as well known as others.
“In some cases, there’s less information about them and fewer studies to support treatments,” he adds.
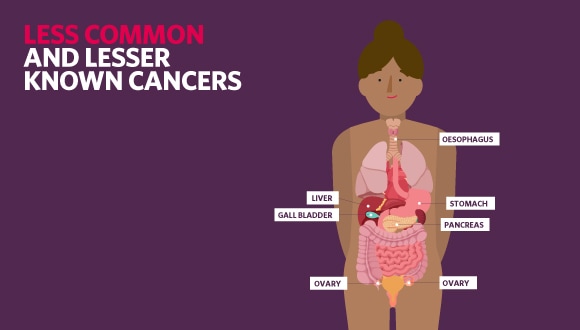
These lesser-known cancers include:
Pancreatic cancer
Pancreatic cancer affects about 4,600 Australians each year and can occur in any part of the pancreas. There are two types of pancreatic cancer: exocrine tumours (about 95% of diagnosed tumours) and neuroendocrine tumours (NETs).
Symptoms rarely show up in the early stages but can include:
- jaundice
- appetite loss
- nausea
- unexplained weight loss
- abdomen or back pain
- diarrhoea or constipation.
Pancreatic NETs have additional symptoms like blurred vision, excessive thirst, increased urination or a spike or drop in blood sugar.
If caught early, treatments can include chemotherapy, radiotherapy and surgery. Surgical removal of the tumour is usually preferred for patients who are otherwise healthy.
If the cancer is in its later stages, treatments for relieving some of the symptoms are usually considered, along with any of the above treatments if possible. Surgeons may insert a stent if there’s a blockage in either the head or tail of the pancreas.
Liver cancer
About 2,800 Australians are diagnosed with primary liver cancer (which means a malignant tumour starts in the liver) each year. It often develops from scarring (cirrhosis) left from fatty liver disease or a long-term hepatitis B or C infection.
Primary liver cancer doesn’t tend to have any symptoms in its early stages. In its later stages or in secondary liver cancer – cancer that has spread to the liver from other organs – symptoms can include:
- tiredness and weakness
- abdomen or shoulder pain
- appetite loss
- nausea
- unexplained weight loss
- jaundice
- pale bowel motions
- abdominal swelling.
Treatment for the disease may include surgery, heat to destroy the tumour (thermal ablation) or chemotherapy. A small number of patients with secondary liver cancer may be able to have surgery to remove the cancer.
Ovarian cancer
Ovarian cancer – of which there are three main types – can affect women in one or both ovaries. More than 1,700 Australian women are diagnosed with ovarian cancer each year, with most patients aged over 50.
Symptoms may include:
- abdominal or pelvic pain
- sudden abdominal swelling, weight gain or bloating
- needing to frequently and urgently urinate
- unexplained weight loss
- feeling full early before finishing a meal.
Ovarian Cancer Australia recommends patients log a symptom diary to track any other unusual symptoms, like changes in bowel habits or unusual bleeding. Treatments involve chemotherapy or surgery – or a combination of both. Sometimes radiotherapy is also used.
Gall bladder cancer
Gall bladder cancer affects more than 800 Australians a year, with more women affected than men. Gall bladder cancer begins in the innermost layer of tissue and spreads through the outer layers as it grows.
There are no symptoms of the disease in its early stages, which makes it difficult to detect. Later-stage symptoms may include:
- vomiting or nausea
- abdominal pain or lump
- jaundice
- fatigue
- fever
- unexplained weight loss.
Treatment options include chemotherapy, radiation therapy or surgery, if the cancer hasn’t spread into other organs.
If the cancer has spread to other organs, palliative treatment will be used to manage the symptoms of the disease.

Oesophageal cancer
More than 1,700 Australians are diagnosed with oesophageal cancer each year, with the average age of diagnosis being 71 years.
Oesophageal cancer develops when abnormal cells grow in the oesophagus, the tube that connects the throat to the stomach.
Symptoms may include:
- heartburn
- persistent reflux
- blood in vomit or stools
- ongoing fatigue
- difficulty swallowing
- abdominal pain, particularly when eating.
Treatment options include chemotherapy and/or radiation therapy to shrink the tumour before surgery.
Stomach cancer
Each year, about 2,580 Australians are affected by stomach cancer, with men almost twice as likely to develop the disease.
While it can affect any part of the stomach, many cases start in the glandular tissue – this is known as gastric cancer. It may not cause symptoms in the early stages, so diagnosis usually happens when the cancer has advanced.
Symptoms may include:
- unexplained weight loss
- difficulty swallowing
- indigestion
- persistent nausea
- a sense of fullness
- abdominal swelling
- fatigue
- blood in vomit or stools.
Treatments include surgery, chemotherapy and radiotherapy – or a combination.
What support is available?
Living with a lesser-known cancer can feel isolating, as care and treatment may not feel so readily available. But there is support out there.
“Rare Cancer Australia is a charity organisation that offers support materials and medical expertise to patients,” says Prof Liauw. “It can also research and advise on suitable clinical trials or potential treatment options.
“Omico offers a similar service, called Comprehensive Genomic Profiling with Australian experts studying cancer at a molecular level to find possible treatments, medications or clinical trials.”
Comprehensive Genomic Profiling detects the individual characteristics – also known as the unique genetic variations – of your cancer so you can get a treatment plan made especially for you based on these findings.
The importance of regular health checks
Looking after yourself is important, and regular health checks can help note any early symptoms.
Free bowel cancer home-testing kits are available for everyone aged 45 to 74. From the age of 50, one of these kits is automatically delivered by mail every two years. You can also ask to be sent one online.
From July 2025, lung cancer screening will be available for eligible people.
BreastScreen Australia invites women aged between 50 and 74 to have a mammogram every two years. Women aged 40 to 49 and over 75 are also able to access free mammograms but don't get a direct invite.
In between checks, listen to your body and look out for any new symptoms – these could be anything from loss of appetite and pain to extreme fatigue.
“If your symptoms aren’t going away with simple measures or they’re getting progressively worse, then you should see your family GP for a review,” says Prof Liauw. “If you’re having specific symptoms that raise red flags, like bleeding from the bowel, you should seek medical advice immediately.”
More support, made easy
Getting a cancer diagnosis can be tough and may leave you feeling overwhelmed. If you’d like another opportunity to ask questions comfortably to gain more information or reassurance around your condition or recommended treatment, we’re here to help. Eligible members can arrange to have a personal discussion with an independent, certified medical specialist at no charge through HCF’s second opinion* service
Related articles
Bowel cancer symptoms: what to look for
Early signs of bowel treatment can go undetected. Here’s how to spot the symptoms, why a bowel cancer screening is so important and what treatment is available.
Ovarian cancer: symptoms, risk factors and treatments
Can ovarian cancer be picked up on a smear test? The answer is no. There's no ovarian cancer test, so knowing the risk factors and symptoms is key.
Cervical cancer symptoms: what to look out for
Cervical cancer is one of the most preventable cancers in the world. By knowing the symptoms, screening and vaccinating, we’re moving closer to elimination.
Is eating soy bad for you?
Is soy a healthy source of protein or does it have health risks? We sort the facts from the fiction, including the best types of soy products to eat.
IMPORTANT INFORMATION
* You must have had hospital cover for 12 months and a specialist consultation to use this service. Excludes Accident Only Basic cover, Extras Only cover and Overseas Visitors Health cover. Conditions apply.
This communication contains information which is copyright to The Hospitals Contribution Fund of Australia Limited (HCF). It should not be copied, disclosed or distributed without the authority of HCF. Except as required by law, HCF does not represent, warrant and/or guarantee that this communication is free from errors, virus, interception or interference. All reasonable efforts have been taken to ensure the accuracy of material contained on this website. It’s not intended that this website be comprehensive or render advice. HCF members should rely on authoritative advice they seek from qualified practitioners in the health and medical fields as the information provided on this website is general information only and may not be suitable to individual circumstances or health needs. Please check with your health professional before making any dietary, medical or other health decisions as a result of reading this website.