3D printing in medicine
With the capacity to generate human body parts, 3D printing may soon revolutionise implant procedures.
Health Agenda magazine
October 2016
In some ways human bodies are like machines. Despite our best efforts they suffer wear and tear – and break down. Replacing machine parts is easy: they are standardised and mass produced. But human bodies are more complicated. Each is unique and often a one-size-fits-all approach doesn’t work.
Fact, not science fiction
Thanks to advances in 3D printing technology, creating what experts call ‘patient specific’ implants, is becoming more achievable. And Australia is leading the way. In the past two years Melbourne-based company Anatomics has collaborated with top surgeons and researchers, both here and overseas, to make patient-specific 3D printed implants for several world-first operations including:
- a polymer cranium for a woman in the Netherlands
- a titanium ankle and heel that allowed a Melbourne man to avoid amputation
- a spine cage implant for a New South Wales woman with deformed lower-back vertebrae
- a titanium sternum and rib implant for a man in Spain.
How does it work?
Andrew Batty, Anatomics’ Chief Executive Officer, says the company has been developing 3D printing for 22 years. “We were one of the first companies in the world to use CT scan imaging to make 3D-printed implants,” he explains.
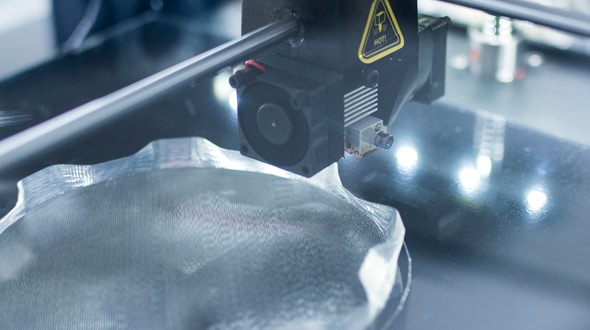
There are a variety of 3D printing technologies but the most frequently used techniques either build an object by applying successive layers of material (similar to an ink-jet printer, but in three dimensions) or use light and/or heat to fuse powdered or liquid material into the desired form. Both metals and polymer plastics are commonly used in medical applications.
The benefits
3D-printed implants offer a number of advantages – using the patient’s own data, gleaned from CT scans, allows implants to fit perfectly. Batty explains that traditional methods of implant construction are casting or milling, both of which are best at producing solid objects. But 3D printing facilitates the creation of specialised ‘internal architecture’, which allows for improved integration with bone and other bodily structures. Plus, implants made this way are light and strong.
In the case of the ankle/heel implant Anatomics made in collaboration with the CSIRO and Professor Peter Choong of Melbourne’s St Vincent’s Hospital, 3D printing was the only way to make an implant light yet strong enough to bear the patient’s weight.
Saving lives – and money
Another bonus is that 3D-printed implants are expected to help reduce the cost of some surgical procedures. “It’s the total cost – in any treatment the hardware is only a small part,” says Professor Gordon Wallace of the University of Wollongong.
Professor Wallace is Executive Research Director of the Australian Research Council Centre of Excellence for Electromaterials Science (ACES) and is working at the leading edge of medical 3D printing. He and his collaborators believe that, as the technology develops, it’ll reduce costs to the health system including:
- less time in surgery
- less likelihood of infection
- more likelihood treatment will be effective.
“What is happening at the moment is 3D printing is being used to deliver solutions to a medical environment where there was no solution,” he adds.
Next generation 3D-printed solutions
Professor Wallace and his team are at the forefront of developing technologies that can print living stem cells and/or other bio-inks, which contain bioactive molecules that can add another layer of effectiveness to a device or increase the efficacy of a procedure.
As Professor Wallace explains, “Bioactives are things like anti-inflammatory drugs or particular proteins or biological molecules that facilitate a regeneration process. For example, they might help certain stem cells turn into cartilage or bone, muscle or nerves, or facilitate nerve regeneration.”
This biochemistry is well known, he says. The key is getting these factors to the right place at the right time. This idea, he explains “is empowered by 3D printing because during the printing process you can distribute those biological molecules where you want them”.
A good example is the cochlear implant ACES researchers are developing that uses 3D printing to integrate anti-inflammatory medication directly into the device. Professor Wallace speculates it’s perhaps five years from being available, depending on regulatory approvals, but says the implications of the technology are wide ranging and go well beyond restoring hearing.
“The cochlear implant electrode is about printing electrodes for stimulation,” he explains. “There are also nerve stimulators in use for epilepsy and Parkinson’s disease, so we’re interested in implantable printed electrodes in general for a range of applications.”
Help for arthritis and diabetes
The ACES team is also working on a collaboration with Professor Choong, dubbed the BioPen. This 3D printing device is designed to help patients regrow cartilage in hips, knees and other often painful joints. As Professor Wallace points out, a clinically approved procedure already exists in which surgeons inject the patient’s own adipose (fat) stem cells into the defective area.
“Sometimes they turn into cartilage, but apparently the efficiency is not high so, in discussions with Professor Choong, we thought if we could create a 3D-printed scaffold that mimics the chemical composition as well as the mechanical properties of cartilage, maybe that would help induce the adipose stem cells into cartilage formation. And it turns out that on the bench it does.”
A surgeon using a BioPen essentially creates a customised implant during an operation, with live bioactivematerials. Again, this technology is not available yet but it will be in the trial stage soon. All going well, it could be helping people with arthritis within five years.
Professor Wallace and the ACES team are also working on developing a system, in tandem with Professor Toby Coates of the Royal Adelaide Hospital, which will use 3D printing to provide a bio support system for islet cells. The goal is to help diabetics produce their own insulin.
We've only just begun
At the very experimental end of the spectrum, in collaboration with researchers at the University of Texas, Dallas, Professor Wallace and his colleagues recently won an Elsevier Atlas Award (for developments that could improve people’s lives). Their innovation: using 3D printing to create an organic, layered structure that resembles human brain matter.
This brain-type structure doesn’t think, but it does work, he says. “We’ve shown it can communicate and send signals. It’s functional.” This last development may seem a little futuristic but, as Professor Wallace makes clear “we’re not just doing experiments for the sake of it”. The goal of this experiment is to provide a safe way to test implant technologies and pharmacological solutions that may help people with neurological diseases.
Asked whether he thinks 3D printing of functioning human organs will be possible in the future, Professor Wallace saysconfidently the answer is yes but there are still challenges. “All these things are platforms that take us towards printed organs,” he says. “But we have to arrange cells, and a blood supply going in and out. That’s a challenge, but not an insurmountable one.”
As to when it might happen, he can’t say. But he does believe that due to the crossover of diverse fields such as stem cell research, bioengineering, 3D printing and medical imaging, things can happen fast.
Ten years ago no one would have thought scientists would be able to replicate brain function. But, as Professor Wallace explains, “Four very significant and mature fields have come together at a point in time when they all benefit from one another. The rate of progress has been quite fast, and I can’t see it slowing down.”